Complex Tibial Plateau Fractures: A Breakthrough Study Compares External Fixation versus Open Reduction and Internal Fixation
Tibial plateaus are critical weight-bearing structures that play a key role in the stability and functionality of the knee joint. Injuries to the tibial plateau can be debilitating and may require orthopedic intervention. Tibial plateau fractures are common accidents that can result from car accidents, falls, and sports injuries.
The treatment of tibial plateau fractures is essential to restore the patient's biomechanical balance, prevent complications, and reduce the likelihood of subsequent degenerative lesions. There are two common surgical options for repairing tibial plateau fractures: external fixation and internal fixation.
External fixation involves the placement of metal pins in the bones above and below the fracture site, followed by the attachment of an external frame to hold the pins and bones together. This technique reduces pain, preserves soft tissues, and allows for swift mobilization while promoting bone healing. However, complications may arise, such as skin irritation, infection, and hardware loosening.
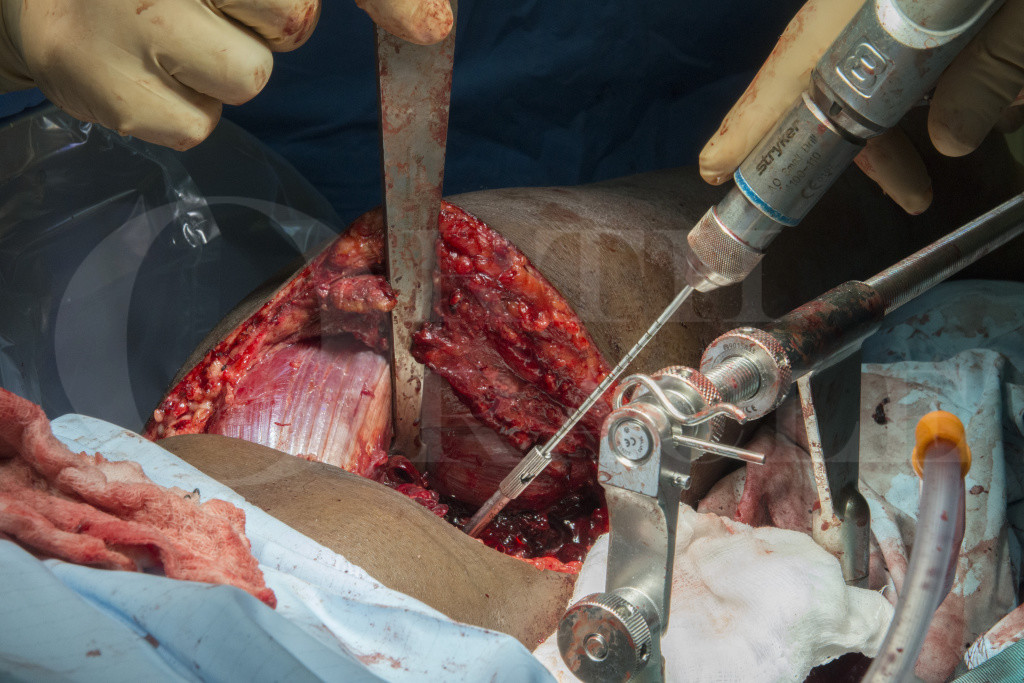
Internal fixation, on the other hand, involves the use of metal screws, plates, or rods placed inside the bone to fixate the fractured pieces. This approach allows for a more stable and anatomical reduction, leading to better functional outcomes. However, internal fixation may lead to soft tissue irritation, screw/bone interface pain, and hardware failure.
Given the pros and cons of both surgical options, there is no clear consensus on the best approach to treating complex tibial plateau fractures. A recent systematic review and meta-analysis aimed to shed light on this topic by comparing the clinical outcomes of external fixation versus open reduction and internal fixation (ORIF) in the management of complex tibial plateau fractures.
The study included five randomized controlled trials and six observational studies, totaling 703 participants. The main outcome measures were functional recovery, radiographic evaluation, complication rates, and reoperation rates. The fractures were classified based on the Schatzker classification system, with type V and VI fractures being considered complex.
The results showed that while both external fixation and ORIF provided satisfactory functional outcomes and fracture union rates, the complication rates and reoperation rates were higher in the ORIF group. Specifically, the ORIF group had a higher risk of implant failure (RR=2.86), intra-articular malreduction (RR=1.84), superficial wound infection (RR=1.68), and deep wound infection (RR=3.3) compared to the external fixation group.

Furthermore, the study found that patients with bicondylar tibial plateau fractures had better outcomes with external fixation than with ORIF. Bicondylar fractures are those that involve both the medial and lateral tibial plateaus and are particularly challenging to manage.
The authors concluded that external fixation may be a better option than ORIF for complex tibial plateau fractures, especially bicondylar fractures. However, further studies are needed to validate these findings and establish clear guidelines for the treatment of these injuries.
As a leading provider of orthopedic implants and instruments, Sichuan ChenAnHui Technology Co., Ltd. is committed to offering high-quality and innovative solutions to meet the needs of orthopedic surgeons and patients. With over 30 Chinese factories and a range of products with a minimum of two years' warranty, the company is well-positioned to provide its customers with procurement, distribution, installation guidance, and after-sales support.
In conclusion, the systematic review and meta-analysis provide valuable insights into the management of complex tibial plateau fractures. The findings suggest that external fixation may be a viable alternative to ORIF, particularly in bicondylar fractures. As always, orthopedic surgeons should carefully evaluate each patient's individual needs and tailor the treatment plan accordingly.